“The use of noninvasive ventilation (NIV) to treat acute respiratory failure is increasing NIV use decreases the rate of endotracheal intubation and mortality in patients with chronic obstructive pulmonary disease (COPD) exacerbations and reduces the rate of endotracheal intubation in patients with cardiogenic pulmonary edema. NIV is commonly used to treat acute respiratory failure on the wards. The benefits of tidal volume (Vte) reduction may be present in critically ill patients without acute respiratory distress syndrome (ARDS).However, an optimal expiratory Vte strategy in NIV for acute respiratory failure has not been well
established, except perhaps in patients with acute hypoxemic respiratory failure. Carteaux et al14 explored the feasibility of a low Vte strategy using NIV in acute hypoxemic respiratory
failure and found that higher Vte was associated with failure defined as need of intubation.”
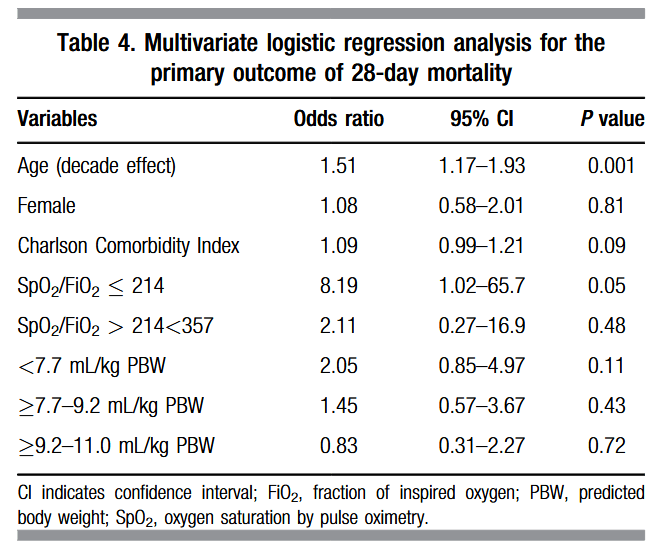
Hayek, A. J., Scott, V., Yau, P., Zolfaghari, K., Goldwater, M., Almquist, J., Arroliga, A. C., & Ghamande, S. (2020). Bedside risk stratification for mortality in patients with acute respiratory failure treated with noninvasive ventilation. Baylor University Medical Center Proceedings, 33(2), 172–177.
Continue reading