Category Archives: Patient Satisfaction
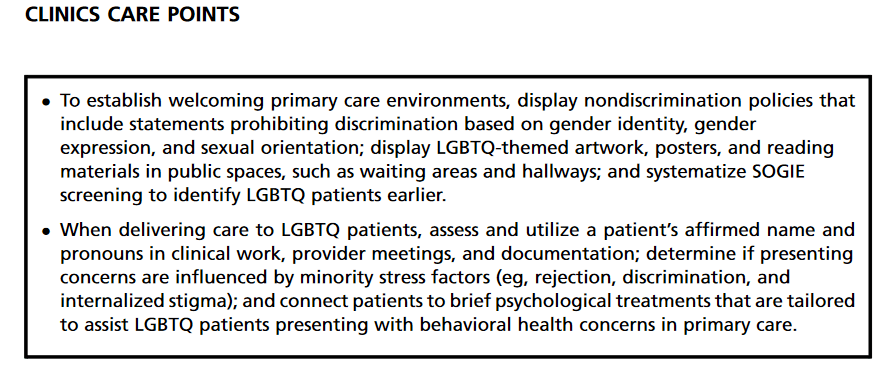
Affirming Care for LGBTQ patients
Rider, G. N., et al (2019). The gender affirmative lifespan approach (GALA): A framework for competent clinical care with nonbinary clients. The international journal of transgenderism, 20(2-3), 275–288.
Earnshaw, V. A., et al (2017). LGBTQ Bullying: Translating Research to Action in Pediatrics. Pediatrics, 140(4)Grasso, C., et al (2019). Planning and implementing sexual orientation and gender identity data collection in electronic health records. Journal of the American Medical Informatics Association, 26(1), 66-70.
Dichter, M. E., et al (2018). Provider perspectives on the application of patient sexual orientation and gender identity in clinical care: a qualitative study. Journal of General Internal Medicine, 33(8), 1359-1365.
Heredia, D., et al (2021). LGBTQ-affirmative behavioral health services in primary care. Primary Care: Clinics in Office Practice, 48(2), 243-257.
Achieving patient satisfaction with discharge instructions
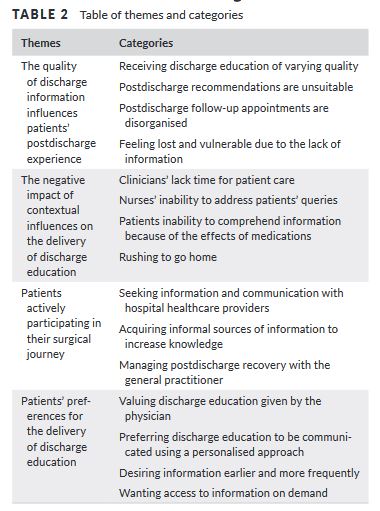
“Discharge education is important for general surgical patients to participate and
regain control of their life after discharge. Overcoming barriers to discharge education is essential to enhance patient comprehension and recollection of the information. Discharge education delivered using a patient‐centred approach provides opportunity to engage patients,
foster patient understanding and enhance patients’ ability to self‐manage and could in turn improve their post-discharge outcomes.” (Kang)
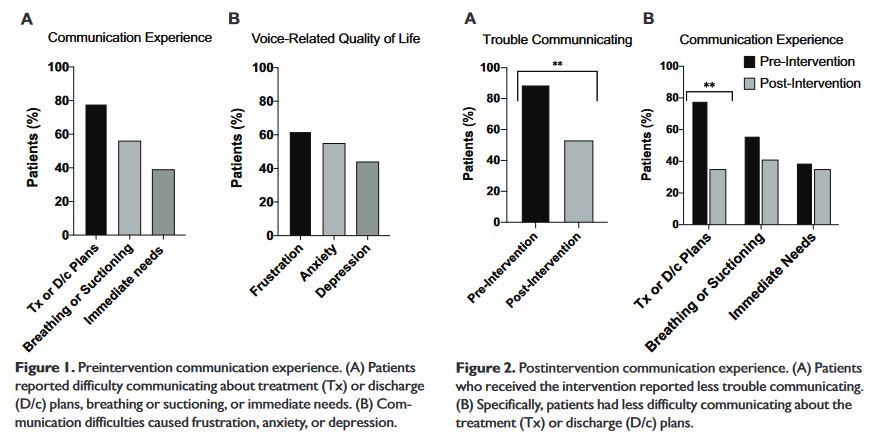
Communicating with intubated or tracheostomy through technology
“Surgical procedures that render patients acutely aphonic can cause them to experience significant anxiety and distress. Participants in this study included hospitalized patients who
acutely lost the ability to speak due to tracheostomy or total laryngectomy. Acute loss of phonation arising from surgery can be highly distressing for patients, and use of augmentative technology may alleviate some of these challenges by improving communication.”
Haring, C., Farlow, J., Leginza, M., Vance, K., Blakely, A., Lyden, T., . . . Casper, K. (2021). Effect of Augmentative Technology on Communication and Quality of Life After Tracheostomy or Total Laryngectomy. Otolaryngology–head and Neck Surgery., 019459982110137.
Full Text for Emory Users
Communication options with patients under isolation precautions: Covid 19
Fang, J., Liu, Y. T., Lee, E. Y., & Yadav, K. (2020). Telehealth Solutions for In-hospital Communication with Patients Under Isolation During COVID-19. The western journal of emergency medicine, 21(4), 801–806. https://doi.org/10.5811/westjem.2020.5.48165
Reengineering the patient’s environment: Establishment of a “Red Box” to improve communications with patients on isolation precautions. (2019). American Journal of Infection Control : Applied Epidemiology in Health Care Settings and the Community, 47(3), 264.
Communication strategies to mitigate fear and suffering among COVID-19 patients isolated in the ICU and their families. (2020). Heart & Lung., 49(4), 344.
Fan, P., Aloweni, F., Lim, S. H., Ang, S. Y., Perera, K., Quek, A. H., Quek, H., & Ayre, T. C. (2020). Needs and concerns of patients in isolation care units – learnings from COVID-19: A reflection. World journal of clinical cases, 8(10), 1763–1766. https://doi.org/10.12998/wjcc.v8.i10.1763
McNairy, M., Bullington, B., & Bloom-Feshbach, K. (2020). Searching for Human Connectedness During COVID-19. Journal of general internal medicine, 1–2. Advance online publication. https://doi.org/10.1007/s11606-020-06082-9
Vilendrer, S., Patel, B., Chadwick, W., Hwa, M., Asch, S., Pageler, N., Ramdeo, R., Saliba-Gustafsson, E. A., Strong, P., & Sharp, C. (2020). Rapid Deployment of Inpatient Telemedicine In Response to COVID-19 Across Three Health Systems. Journal of the American Medical Informatics Association : JAMIA, 27(7), 1102–1109. https://doi.org/10.1093/jamia/ocaa077
Missed nursing care and the impact on patient and hospital outcomes
Impact of Patient Safety Culture on Missed Nursing Care and Adverse Patient Events. (2019). Journal of Nursing Care Quality., 34(4), 287.
(2018). Journal of Clinical Nursing., 27(11-12), 2248.
Does Missed Care in Isolated Rural Hospitals Matter? (2018). Western Journal of Nursing Research., 40(6), 775.
The association between nurse staffing and omissions in nursing care: A systematic review. (2018). Journal of Advanced Nursing., 74(7), 1474.
Impact of Patient Safety Culture on Missed Nursing Care and Adverse Patient Events. (2019). Journal of Nursing Care Quality., 34(4), 287.
A research protocol for testing relationships between nurse workload, missed nursing care and neonatal outcomes: The neonatal nursing care quality study. (2015). Journal of Advanced Nursing., 71(3), 632.
Practice environment characteristics associated with missed nursing care. (2018). Journal of Nursing Scholarship : An Official Publication of Sigma Theta Tau International Honor Society of Nursing /, 50(6), 722.
Development and validation of the MISSCARE survey—Pediatric version. (2018). Journal of Advanced Nursing., 74(12), 2922.
Missed care: A need for careful ethical discussion. (2018). Nursing Ethics., 25(5), 549.
Nursing work engagement and patient/hospital outcomes
Stevanin, S., Palese, A., Bressan, V., Vehviläinen-Julkunen, K., & Kvist, T. (n.d.). Workplace-related generational characteristics of nurses: A mixed-method systematic review. Journal of Advanced Nursing., 74(6), 1245-1263.
Lui, J., Andres, E. B., & Johnston, J. M. (2018). Presenteeism exposures and outcomes amongst hospital doctors and nurses: a systematic review. BMC health services research, 18(1), 985.
Zadvinskis, I., Carr, J., Schweitzer, K., Patil, N., Clifton, W., & Ebert, K. (2019). The Impact of Nursing Work and Engagement on Patient Falls. Journal of Nursing Administration., 49(11), 531-537.
Bogaert, P. V., Heusden, D. V., Slootmans, S., Roosen, I., Aken, P. V., Hans, G. H., & Franck, E. (2018). Staff empowerment and engagement in a magnet® recognized and joint commission international accredited academic centre in Belgium: a cross-sectional survey. BMC health services research, 18(1), 756.
Lui, J., & Johnston, J. M. (2019). Working while sick: validation of the multidimensional presenteeism exposures and productivity survey for nurses (MPEPS-N). BMC health services research, 19(1), 542. https://doi.org/10.1186/s12913-019-4373-x
Flanders, S., Hampton, D., Missi, P., Ipsan, C., & Gruebbel, C. (n.d.). Effectiveness of a Staff Resilience Program in a Pediatric Intensive Care Unit. Journal of Pediatric Nursing., 50, 1-4.
Saito, Y., Igarashi, A., Noguchi-Watanabe, M., Takai, Y., & Yamamoto-Mitani, N. (n.d.). Work values and their association with burnout/work engagement among nurses in long-term care hospitals. Journal of Nursing Management., 26(4), 393-402.
Ding, B., Liu, W., Tsai, S. B., Gu, D., Bian, F., & Shao, X. (2019). Effect of Patient Participation on Nurse and Patient Outcomes in Inpatient Healthcare. International journal of environmental research and public health, 16(8), 1344.
Tomietto, M., Paro, E., Sartori, R., Maricchio, R., Clarizia, L., De Lucia, P., . . . Finos, R. (n.d.). Work engagement and perceived work ability: An evidence-based model to enhance nurses’ well-being. Journal of Advanced Nursing., 75(9), 1933-1942.
Wan, Q., Zhou, W., Li, Z., & Shang, S. (2018). Associations of Organizational Justice and Job Characteristics with Work Engagement Among Nurses in Hospitals in China. Research in Nursing & Health., 41(6), 555-562.
Havens, D., Gittell, J., & Vasey, J. (n.d.). Impact of Relational Coordination on Nurse Job Satisfaction, Work Engagement and Burnout: Achieving the Quadruple Aim. Journal of Nursing Administration., 48(3), 132-140.
Olender, L., Capitulo, K., & Nelson, J. (n.d.). The Impact of Interprofessional Shared Governance and a Caring Professional Practice Model on Staff’s Self-report of Caring, Workplace Engagement, and Workplace Empowerment Over Time. Journal of Nursing Administration., 50(1), 52-58.
Dempsey, C., & Assi, M. (n.d.). The Impact of Nurse Engagement on Quality, Safety, and the Experience of Care: What Nurse Leaders Should Know. Nursing Administration Quarterly., 42(3), 278-283.
Santos, A., Chambel, M., & Castanheira, F. (n.d.). Wellbeing among hospital nurses: A cross-sectional study of the contributions of relational job characteristics. International Journal of Nursing Studies., 105, 103438.
Deetz, J., Davidson, J., Daugherty, J., Graham, P., & Carroll, D. (n.d.). Exploring correlation of nurse manager meaning and joy in work with employee engagement. Applied Nursing Research., 151297.
Schirle, L., & Dietrich, M. (n.d.). Advanced practice registered nurses’ work environment perceptions in hospitals: A cross-sectional survey. Journal of Nursing Management., 28(4), 919-926.
