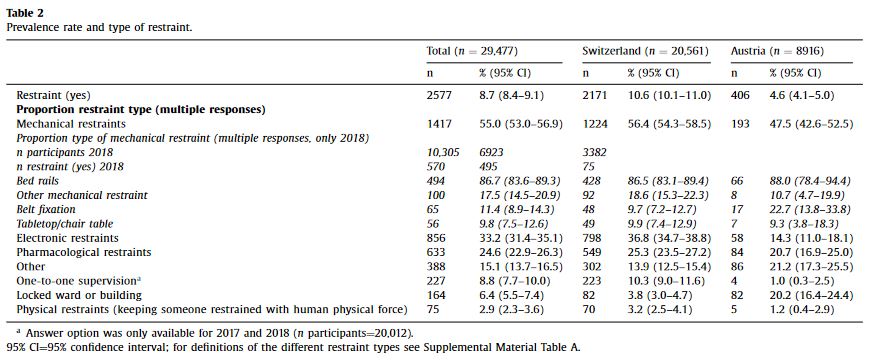
“Restraints are likely to negatively affect patients’ health and therefore a reduction in their usage is recommended for all health-care settings. To date, research on restrictive practices has concentrated on mental health and long-term care settings. To ensure restraints are used as little as possible in the acute-care hospital setting, it seems important to investigate more comprehensively the use of restraints, to include all types of restraints irrespective of ward type or subpopulations and to identify factors associated with restraint use. Restraints are often utilised in hospitals in complex care situations such as with patients at risk of falling or with delirium. When using restraints the consideration of processes like documentation and evaluation shows great potential for improvement. Standardisation of these processes and education of the interprofessional team could be beneficial for raising awareness and for the sustainable reduction of restraint use.”
Thomann, S., Zwakhalen, Richter, Bauer, & Hahn. (2021). Restraint use in the acute-care hospital setting: A cross-sectional multi-centre study. International Journal of Nursing Studies,114, 103807.
Continue reading