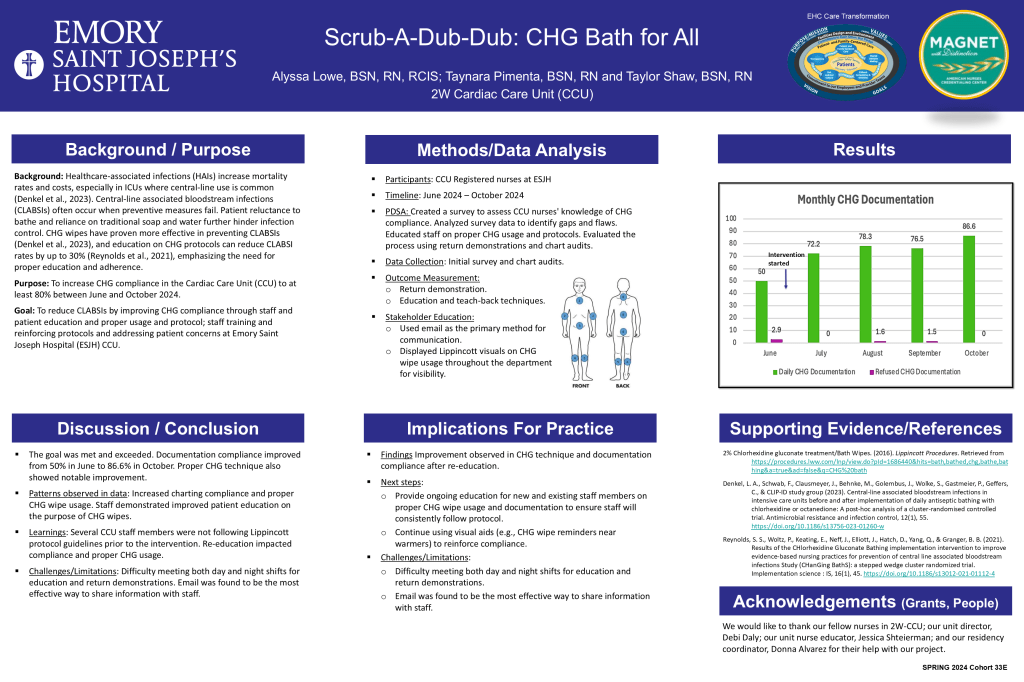
Category Archives: EHC Nurse Residency Posters
BedSide Shift Report (BSSR): Counting Everyone In
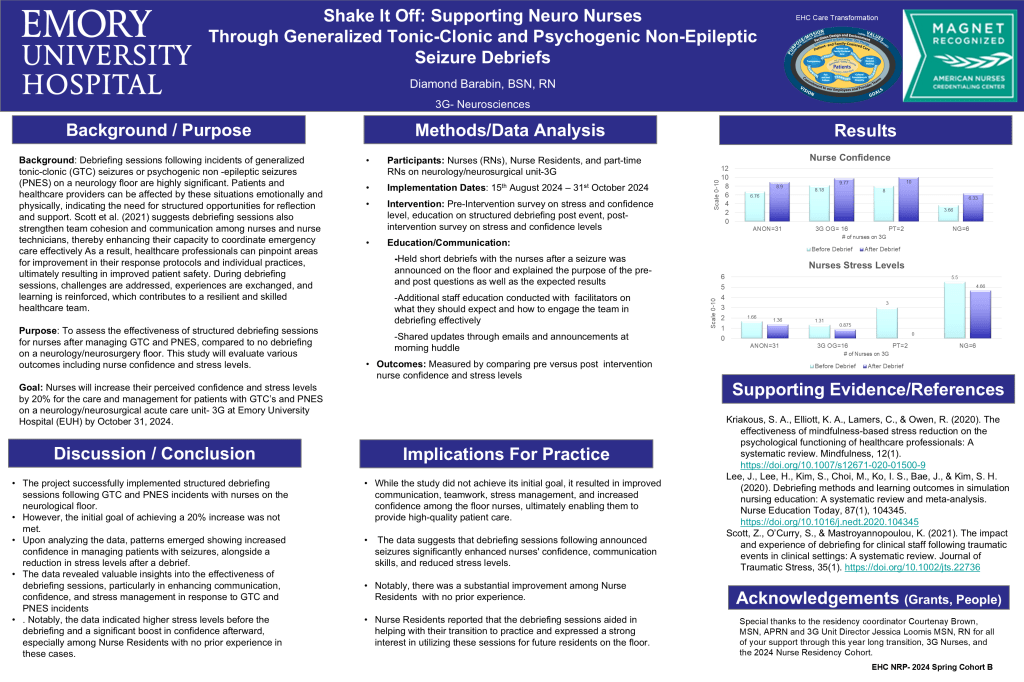
: Emory Saint Joseph’s Hospital (ESJH) has maintained its Magnet designation for the seventh consecutive year, reflecting its commitment to exceptional patient care, safety, and satisfaction (Emory Healthcare, 2024). Bedside shift reports (BSSR) are crucial in ensuring safe continuity of care, improving patient outcomes such as reduced falls and medication errors, and enhancing the overall patient experience (Wong, 2023). This practice promotes patient safety by identifying errors and avoiding delays or injuries while fostering clear communication and patient-centered care that aligns with individual needs and preferences (Jimmerson et al., 2021; Wong, 2023).
Gloria Cruz, BSN, RN and Oulimata Simal, BSN, RN 3West Interventional Cardiology/3E Heart Failure Unit BedSide Shift Report (BSSR): Counting Everyone In [Emory Healthcare Nurse Residency] Emory Saint Joseph’s Hospital, Atlanta GA
From Push to Pod: NICU Handoffs That Deliver

“Effective communication during handoffs from Labor and Delivery (L&D) to the Neonatal Intensive Care Unit (NICU) is critical, especially in managing high-risk cases immediately following birth. However, current handoff practices often lack standardization and omit essential information, which can impede accurate assessments and timely interventions by both L&D and NICU teams. These inconsistencies compromise neonatal team preparedness and contribute to communication failures, a factor in over 70% of sentinel events (Helen et al., 2018). Brewer et al. (2023) highlight the importance of enhancing handoff workflows to improve preparedness. Evidence shows that streamlined handoff processes foster better communication, collaboration, and critical thinking among L&D and NICU staff, ultimately enhancing patient safety and care outcomes.”
Lauren Deese, BSN, RN (NICU) and Cassidy Valbrun, MN, RN (L&D) Women’s Services From Push to Pod: NICU Handoffs That Deliver [Emory Healthcare Nurse Residency] Emory Saint Joseph’s Hospital, Atlanta GA
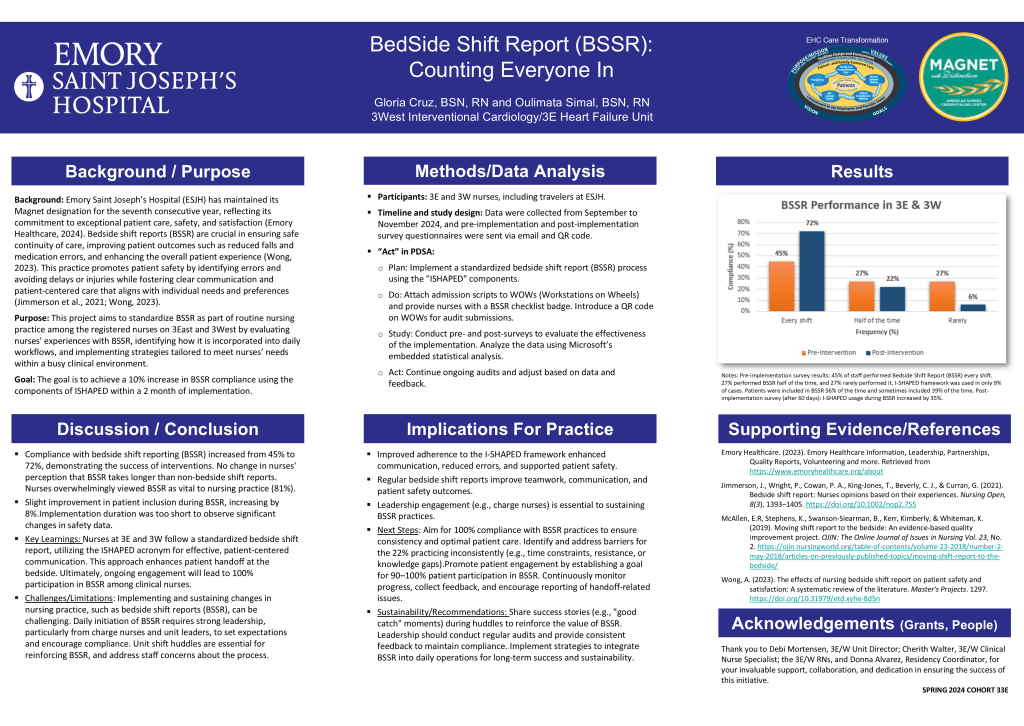
Breathing Better: Enhancing IS Compliance through Nursing Interventions
“Patients undergoing surgery, particularly those with pre-existing respiratory conditions or chest tubes, face a high risk of postoperative pulmonary complications, such as hypoxia and pneumothorax, which can prolong hospital stays and worsen outcomes (Dhillon et al., 2023). The incentive spirometer (IS), a non-invasive tool designed to encourage deep breathing and lung expansion, effectively prevents such complications. However, adherence to IS use is often hindered by insufficient patient education and inconsistent reminders. Studies suggest that interactive tools like checklists and reminder systems can significantly improve IS engagement and documentation (Kneuertz et al., 2020; Pangborn et al., 2020).”
Winifred Afu, BSN, RN; Anna Gabriel, BSN, RN; Somi Kim, MN, RN and Sarah Muh, BSN, RN (2 South CV Stepdown); Jennifer Nguyen MN, RN and Teaira Yates, BSN, RN (5 East/West Internal Medicine Breathing Better: Enhancing IS Compliance through Nursing Interventions [Emory Healthcare Nurse Residency] Emory Saint Joseph’s Hospital, Atlanta GA
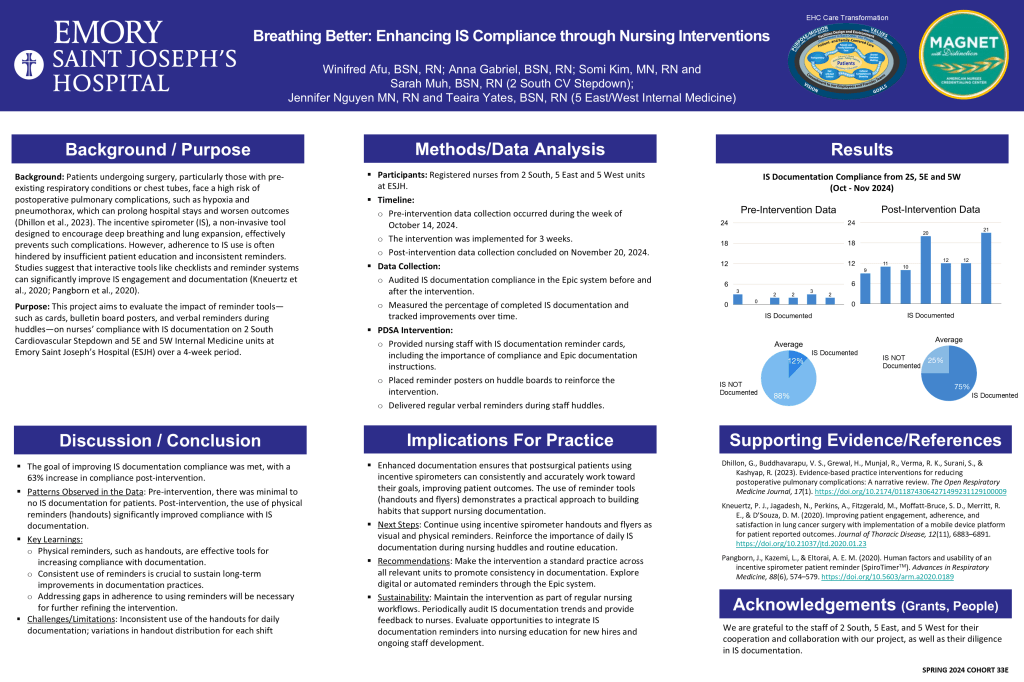
Scrub-A-Dub-Dub: CHG Bath for All
“Healthcare-associated infections (HAIs) increase mortality rates and costs, especially in ICUs where central-line use is common (Denkel et al., 2023). Central-line associated bloodstream infections (CLABSIs) often occur when preventive measures fail. Patient reluctance to bathe and reliance on traditional soap and water further hinder infection control. CHG wipes have proven more effective in preventing CLABSIs (Denkel et al., 2023), and education on CHG protocols can reduce CLABSI rates by up to 30% (Reynolds et al., 2021), emphasizing the need for proper education and adherence.”
Alyssa Lowe, BSN, RN, RCIS; Taynara Pimenta, BSN, RN and Taylor Shaw, BSN, RN 2W Cardiac Care Unit (CCU) Scrub-A-Dub-Dub: CHG Bath for All [Emory Healthcare Nurse Residency] Emory Saint Joseph’s Hospital, Atlanta GA
Code Clear Communication: ORchestrated Dialogue: Streamlining OR Communication for Professional Excellence.
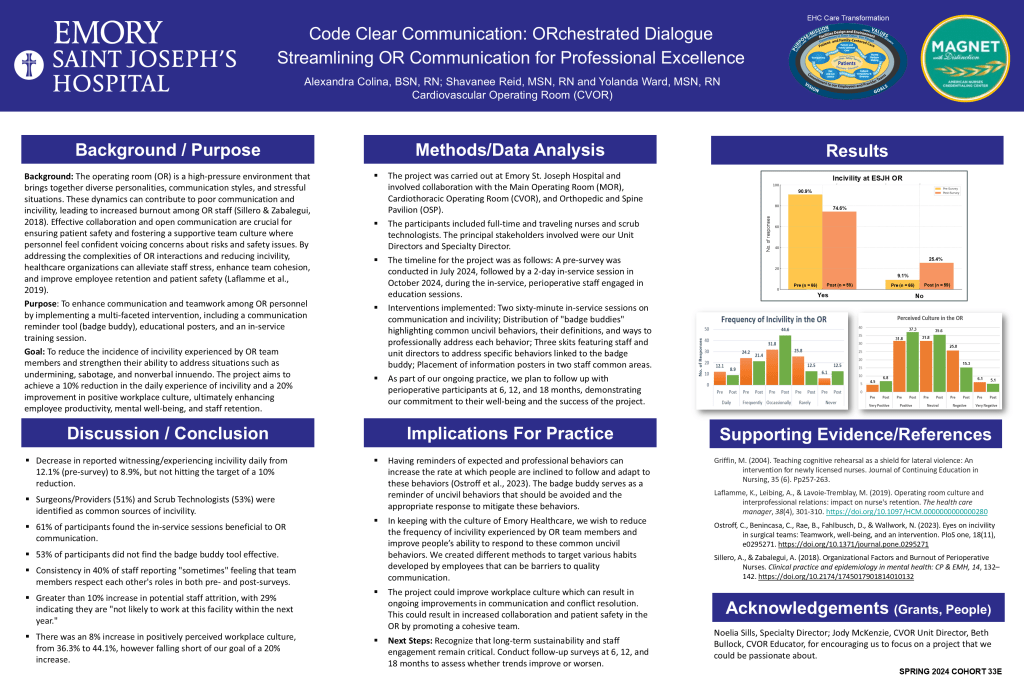
“The operating room (OR) is a high-pressure environment that brings together diverse personalities, communication styles, and stressful situations. These dynamics can contribute to poor communication and incivility, leading to increased burnout among OR staff (Sillero & Zabalegui, 2018). Effective collaboration and open communication are crucial for ensuring patient safety and fostering a supportive team culture where personnel feel confident voicing concerns about risks and safety issues. By addressing the complexities of OR interactions and reducing incivility, healthcare organizations can alleviate staff stress, enhance team cohesion, and improve employee retention and patient safety (Laflamme et al., 2019).”
Alexandra Colina, BSN, RN; Shavanee Reid, MSN, RN and Yolanda Ward, MSN, RN Cardiovascular Operating Room (CVOR) Code Clear Communication: ORchestrated Dialogue: Streamlining OR Communication for Professional Excellence [Emory Healthcare Nurse Residency] Emory Saint Joseph’s Hospital, Atlanta GA

