“Nurse recognition has been viewed as a critical component of a healthy work environment. The American Association of Critical-Care Nurses (AACN) describes elements of meaningful recognition, including a formal process from the organization that has structured and
sustainable processes for recognizing the contributions of individuals. In this sense, meaningful recognition includes identifying and honoring the value a nurse brings to the organization. Nurses who feel recognized have higher compassion satisfaction and lower burnout and describe feelings of gratitude, respect, and appreciation from their patients.” (Joseph)
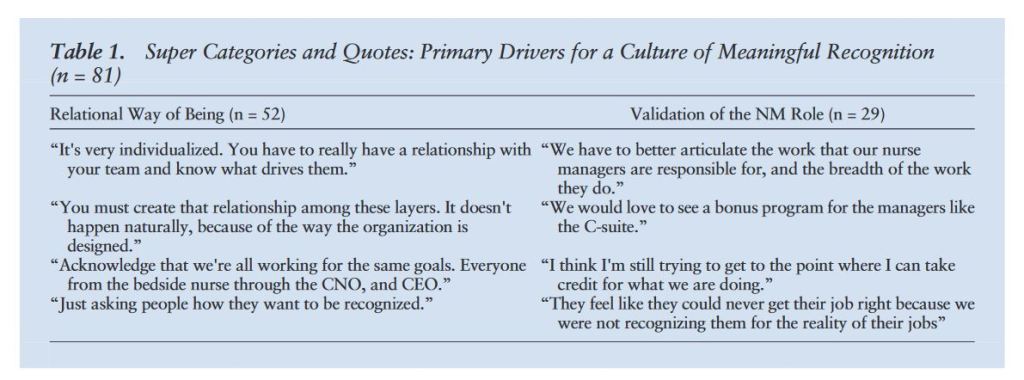
Joseph, M. L., Kelly, L., Davis, M. B. H., Zimmermann, D., & Ward, D. (2023). Creating an Organizational Culture and Climate of Meaningful Recognition for Nurse Managers. JONA: The Journal of Nursing Administration, 53(7/8), 370–377
Continue reading