Author Archives: John
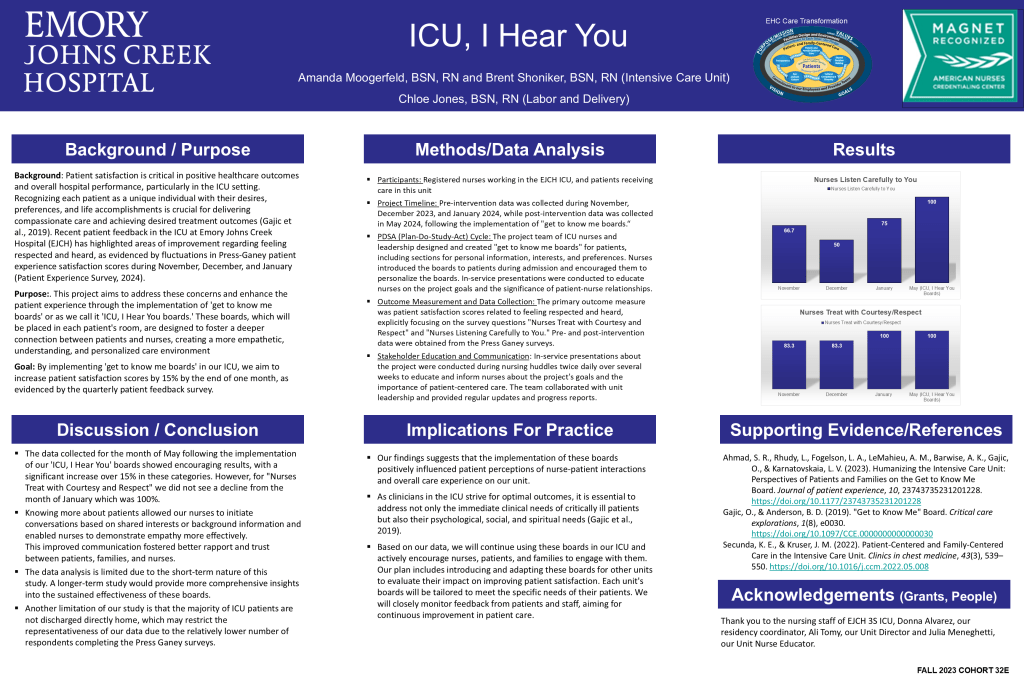
Nurse Residency Posters: ICU, I Hear You
Weight based dosing in the ICU
“Propofol and dexmedetomidine are sedative agents used in the intensive care unit (ICU) for patients requiring mechanical ventilation along with fentanyl that has both analgesic and
sedative properties. It has also been shown decreasing overall sedation by implementing
daily interruption of sedative infusions decreased duration of MV and ICU length of stay (LOS). However, there is a lack of data regarding patient’s weight that may play an impact on dosing of sedation.”
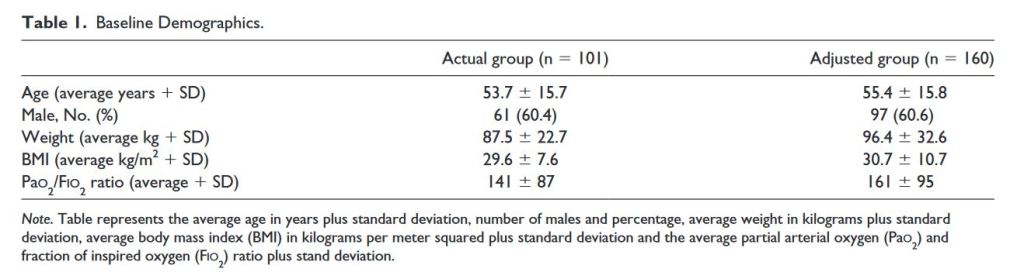
Yeary, J.,et al (2020). Adjusted vs Total Body Weight-Based Dosing of Sedation and Analgesia Used in the Intensive Care Unit. Hospital Pharmacy, 55(6), 400–404.
Continue readingEmory Authors: Looking Back to Advance Equity in Psychiatric Nursing: Strategies for the Classroom and for Practice.
“With deep historical roots in psychiatry, structural racism persists in psychiatric nursing today. Psychiatric nurses may hold implicit biases and stereotypical beliefs that influence how they perceive, assess, and interact with people from different racial backgrounds, leading to discrimination, poor treatment, and misdiagnosis. To eliminate discrimination in clinical care and diversify the workforce, there is an urgent need to integrate teaching and learning strategies that address influences of racism and racial identity in psychiatric nursing education. This article explores the historical context and proposes antiracist psychiatric nursing teaching and practice interventions to reduce the harms of racism.”
“Since the late 19th century, psychiatric nursing evolved in tandem with American psychiatry and inherited many of the same biases. From the mid-19th century on, psychiatric care was
provided in racially segregated facilities, which limited the ability of Black women to become nurses and severely impacted patient care (Smith, 2020). Black nurses fought to be able to undertake mental health training and provide psychiatric practice but were restricted to Black-only hospitals, such as the Tuskegee Veterans Affairs hospital in Alabama, which provided psychiatric care to Black returned service men and the local community. In adopting the principles of mainstream psychiatry, psychiatric nursing also adopted a program of “mental hygiene” and eugenic science.”
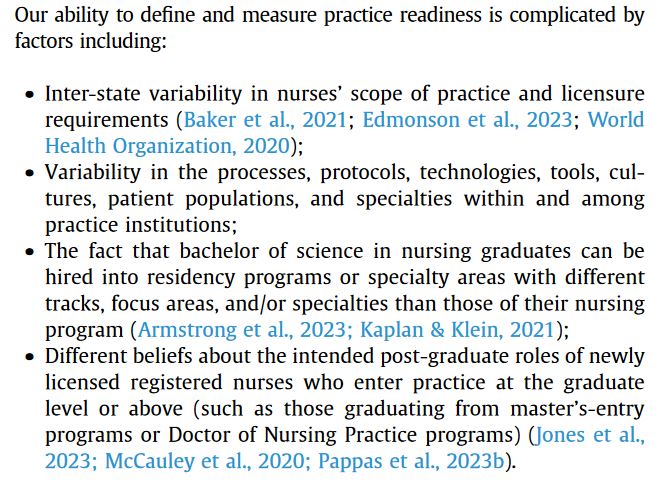
Emory Authors: Reject the “Practice Readiness Myth”
“The nursing profession is engaged in robust national dialogue on how to implement competency-based education. This dialogue often conflates the concept of “competency-based education” with nursing “competence” or “practice readiness.” Our aim is to discuss the potential harms of conflating “competency-based education” with “competence” or “practice readiness.” This commentary explores the possible risks of issue conflation. Risks include (a) suggesting that nurses who have successfully obtained licensure are not “competent” or “ready to practice,” and (b) de-emphasizing the importance of safe and sustainable work environments for new graduate nurses. We discuss the need to separate conversations about “competency-based education” and “practice readiness”; the need to increase the clarity and specificity of discourse surrounding competency-based education; and the need for strategic alignment across academia and practice.”
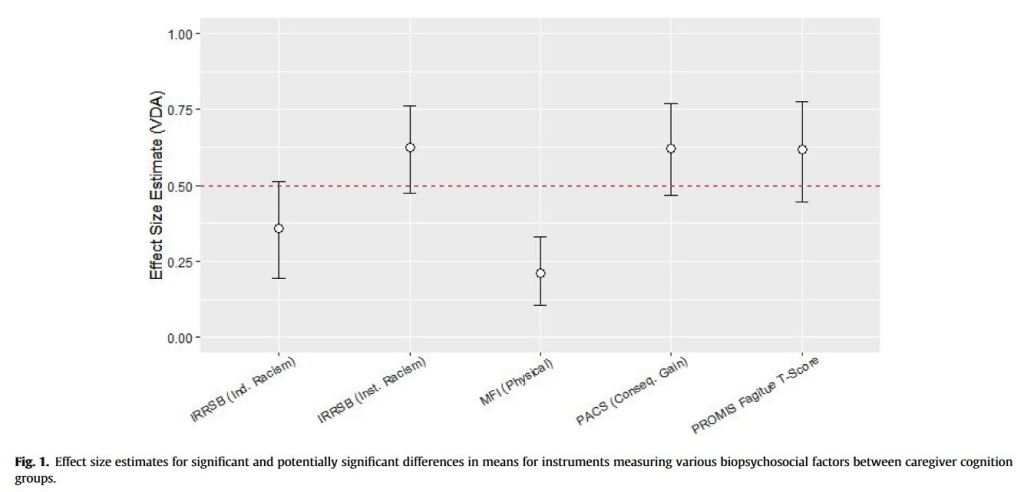
Emory Authors: Factors related to cognitive performance among black caregivers of persons living with a chronic illness: An exploratory study
“While several studies have investigated the impact of informal caregiving on physical and mental health outcomes, there is a gap in the literature concerning the effect of caregiving on cognitive performance, an essential component of independent living and caregiving. The limited research to date predominantly suggests that informal caregiving increases the risk of cognitive impairment and even dementia. This increased risk is related to the stress and
poor sleep associated with the caregiving role, along with various psychosocial, behavioral, and physiological factors that negatively impact caregivers.”
“Despite the increased risk that caregivers have for cognitive impairment, to our knowledge, no studies to date have examined caregiving and cognitive performance among Black caregivers. Black caregivers are the second largest population of caregivers in the U.S.
They face systemic inequities that result in unique challenges and stressors which affect their caregiving roles and compound negative health outcomes. Black caregivers are also more likely to have lower household incomes, experience financial hardship, and are less likely to self-report good physical health.”
Intrahospital Transfers
“Intra-hospital handover requires clear processes, to promote high-quality information sharing. Ensuring these processes are broad and acceptable across units may ensure nurses’ needs are met. Relational continuity between nurses is an important consideration when improving intra-hospital handover.”
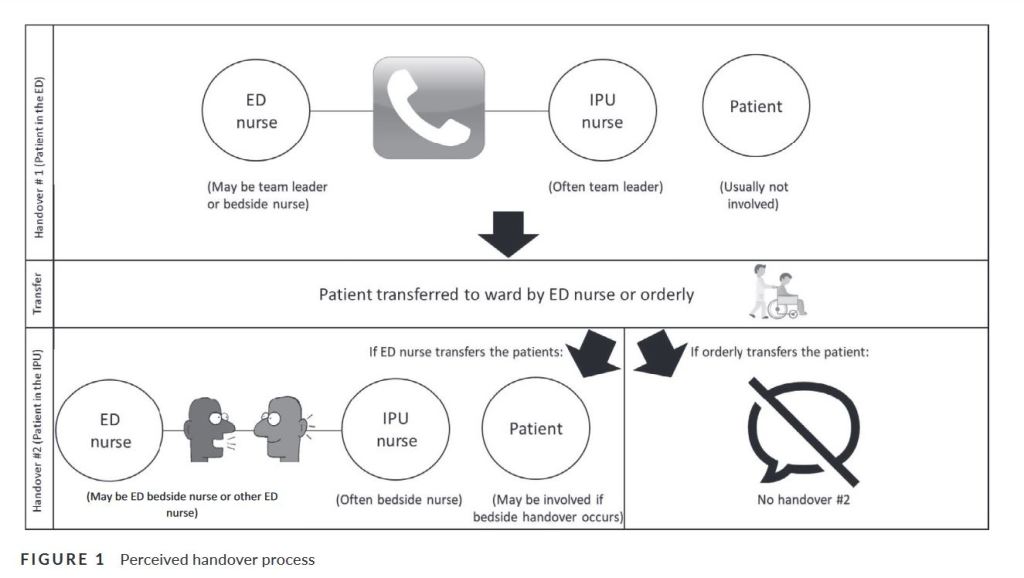
“Improvement in intra-hospital handover is challenging because multiple hospital units are involved. A meso-level leader could liaise across units and standardise handover processes using SOPs. Within SOPs, checklists could support standardisation consisting of broad content that is acceptable to end-users across varying units, which could be incorporated into EMR. Acknowledging handover as a high-risk task and giving nurses permission to spend time preparing for handover may also facilitate high-quality handover.”
Tobiano, G., et al. (2020). Front‐line nurses’ perceptions of intra‐hospital handover. Journal of Clinical Nursing (John Wiley & Sons, Inc.), 29(13/14), 2231–2238.
Continue reading